Summer '24 Retreat: Scaling Primary Care
XPC Course: Utilizing Pharmacists in Primary Care is launching in August! 💊
XPC Retreats bring together thoughtful people to have candid conversations about hot topics in primary care. Healthcare conversations frequently face the Blind Men and an Elephant problem which we solve by making sure our retreat gatherings feature those from various healthcare silos (insurance, clinicians, brokers, health tech, private equity, etc.) who may not otherwise have the chance to speak freely with each other. The theme of our recent summer retreat was “Scaling Primary Care,” inspired by Dr. Eric Bricker of AHealthcareZ. He was kind enough to feature his takeaways in one of his famous white board videos. We share our own summary of the event with more detailed notes from the event for our paid subscribers, including thoughts from Gus Roman who helped us with organization and partnerships during our planning.
First, a big thank you to Aasim Saeed, MD, MPA of Amenities Health, Kike Oduba, MD, MPH of WellnessWits and MassChallenge for supporting our event through sponsorship! As we look forward to future retreats, we are open to suggestions for future themes and welcome working with sponsors who like what we do and want to team up with us.
Paying for primary care
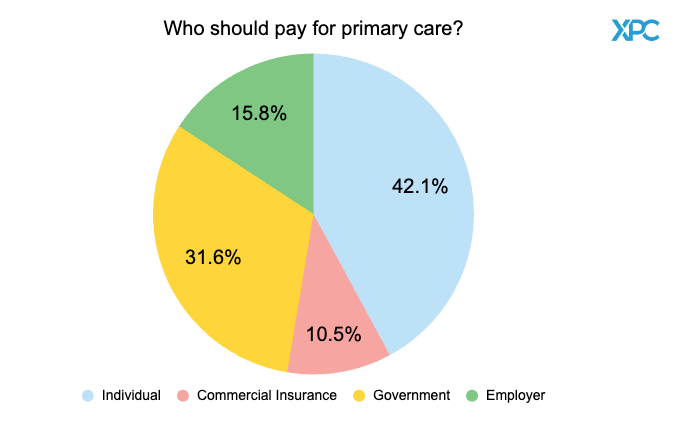
To stimulate and guide conversation throughout the retreat, we polled attendees on relevant issues. Scaling primary care requires obtaining patients and patients currently receive primary care from different payers. We first asked “Who should pay for primary care?”
Results reflected an overall belief that patients had the most to gain when taking charge, by way of payment, of their own primary care. Many of the current problems with the primary care system comes from misalignment of long term incentives when paid by third parties (a topic we cover in our Primary Care 101 course). Commercial insurance and employers only have incentives to keep patients healthy for a span of several years based on how frequently people change jobs and plans on average, but the government has an incentive to keep citizens healthy across their lifespan. One major difficulty brought up, among many, for the government to take over primary care payment was the fragmentation of the US government and uncertainty about which level (locality to federal) would take responsibility for payment and management of primary care. Those who picked employer and commercial insurance made a case about practicality based on how the health system exists today. Over half of Americans are covered under some form of employer sponsored or commercial insurance and this paradigm is unlikely to change any time soon.

Patient acquisition markets
Many of our attendees were operators and clinicians. We wanted to see how they approached finding new patients for their services, so we asked “What is the best market for patient acquisition?”
The responses suggest a bullish attitude towards the direct to consumer market, but conversation reflected otherwise. Different government models were discussed with some attendees having participated in CMMI models. Across the board, everyone appeared to agree that government programs have too many requirements and often fail to pay appropriately. Employers came next in discussion and, unlike the general distaste for government programs, just about everyone agreed on the potential for scale in the employer market. During the conversation about best markets, the impact of primary care came under scrutiny. Examples like employee wellness programs, which have had barely any impact on health or finances, were highlighted to question the validity of selling primary care. Ultimately, the discussion resolved with an agreement that different markets have different needs.
The role of the PCP
On the other side of scaling is the supply of providers. We first wanted to see how people felt about the role of the primary care provider (PCP). “Is the role of the PCP primarily as a delegator/communicator or a ‘one stop shop’?”
Most of the immediate conversation after each poll question involved a bit of litigation about the wording and being forced into picking a single answer for complicated questions. This question raised more dissent than the others as most believed PCPs should participate equally in care navigation and medical care. But this line of dialogue was as fleeting as it was intense. The subsequent conversation tried to navigate the dichotomy and touched on a few interesting topics along the way.
PCP as Delegator (aks “referralist”)
In large cities and integrated payvider systems, referrals happen with ease and often with surprisingly helpful tech. References to the common analogy of PCP as quarterback came out during this section and the idea was raised of PCP as a “first stop shop” rather than a “one stop shop.” However, one attendee brought up the reality that most PCPs are referralists in hospital systems. Many of the clinicians brought up concerns around physicians having to see higher numbers of patients, forcing them to refer more than necessary. One participant mentioned people may not want to even attend medical school if they knew their future was simply to delegate care.
PCP as “One Stop Shop”
The qualification “one stop shop for what you need most of the time” was more widely accepted than the moniker “one stop shop.” Different locations and stages of life require different expertise and local PCPs will always end up specializing to their population. Not to mention PCP as a one stop shop seems disingenuous when most PCP offices will carve out certain services such as mental health, vaccines, etc. Building trust lies at the core of the one stop shop conversation and a brief aside about tech came to an agreement that tech will always only augment the PCP because people will want a trusted person to confirm their chatbot/Google search/AI response.
Primary Care and Medical Education
Certain tough points surfaced about medical education. Medical schools might be attracting the wrong people. People in the medical field propagate the myth of an obsolete physician archetype which prospective students seek to be when applying only to get disillusioned as their education progresses. Part of the issue comes from the knowledge base learned in school often not matching knowledge and skills needed in practice. PCPs start practicing in a largely administrative specialty without the proper administrative tools or training. Academic health centers came under fire as education in that default setting innately funnels students into hospital-based jobs, which often are the referral mills described earlier.
Other Team Members
Nurse practitioners came up only briefly when discussing hospital systems beginning to replace physicians as PCPs. Pharmacists took center stage throughout the primary care team discussion. All the physicians had positive views of pharmacists they work with and have relied on their expertise in one way or another. Through bits and pieces of disparate stories about encounters with pharmacists, the group learned that pharmacists can do more than anyone individually thought, including patient education and, in some states, independently prescribing or refilling medications. Many of the operators and clinicians stated they would hire a pharmacist if their practices only had the budget to add one more person.
Relationship with hospitals and health systems
Hospitals did not have friends in the room during this section. The 10.5% dissent reflected more of a difference in understanding the question. They read the question as “primary care should interact with hospitals” rather than “primary care should be owned and operated by hospitals.” Those who worked in hospital leadership offered up ways their hospital systems have implemented ACOs which supported primary care and ways systems have improved primary care quality and standardization. Everyone else countered with the misaligned incentives arising from hospitals relying on high reimbursement specialties for income while leaning on primary care as loss leaders incentivized to generate referrals into the system.
Financial models of the future
Today’s primary care financing landscape allows three main models of sustainability to exist: direct to consumer (individual or employer DPC), value based contracting (in all its many forms), and loss leader to refer to lucrative procedures and specialties (current hospital model). Those who chose the downstream referral model were skeptical at how quickly the healthcare system would change based on how slow it has historically responded to changes. Several participants brought up stats on the growth of VBC and DPC which affirmed the rest of the group’s optimism in seeing either model dominate in the next 20 years. VBC contracting is largely driven by government payer mandates and features mostly hospital systems but has been trending towards including smaller groups and practices (e.g. ACO Primary Care Flex Model). The spread of DPC has been primarily driven by growth in the employer market.
Having a PCP
Healthcare tends to be a “do as I say and not as I do” field. In a room full of healthcare leaders and innovators, only about half reported to have their own PCP. The results were met with some shock and some amusement, though in other events we’ve hosted, around 50% seems to be a standard percentage. Discussion after this question navigated around what having a PCP means. Some people treat companies as their PCP rather than individuals and others, namely those with chronic or rare disease, will use their specialist as a PCP. There was also a tangent about preventative medicine and what insurance will cover, but before the conversation devolved into clinicians arguing over population health and number needed to treat, we brought the focus back to care delivery. The individuals from the insurance companies talked about the difficulty of having their covered lives engage with PCPs as well as the messy process of PCP attribution and assignment.
Our article continues for paid subscribers with highlights of additional discussion topics: the evolving role of urgent care centers and an investor’s perspective on scaling primary care plus bonus quotes from hallway conversations.