Utilizing Pharmacists in Primary Care
Learn how to unlock the potential of interdisciplinary care
Clinical expertise of community pharmacists is highly underutilized in primary care. We put together a course to highlight the capabilities of pharmacists to supercharge primary care teams through improved care ops, increased revenue, and better patient outcomes. Here’s the breakdown of our curriculum:
Session 1: Opportunities in Primary Care
Session 2: Pharmacist Education and Training
Session 3: Optimizing Therapy
Session 4: Clinical Superpowers
Session 5: Pharmacist Care Operations
Session 6: Metrics and Outcomes
Session 7: Paying Pharmacists
Session 8: Pharmacist Scope of Practice
Session 9: Legislative Landscape for Pharmacists
Session 10: Integrating Pharmacists
MEET THE INSTRUCTORS
SELECTED HIGHLIGHTS FROM THE COURSE
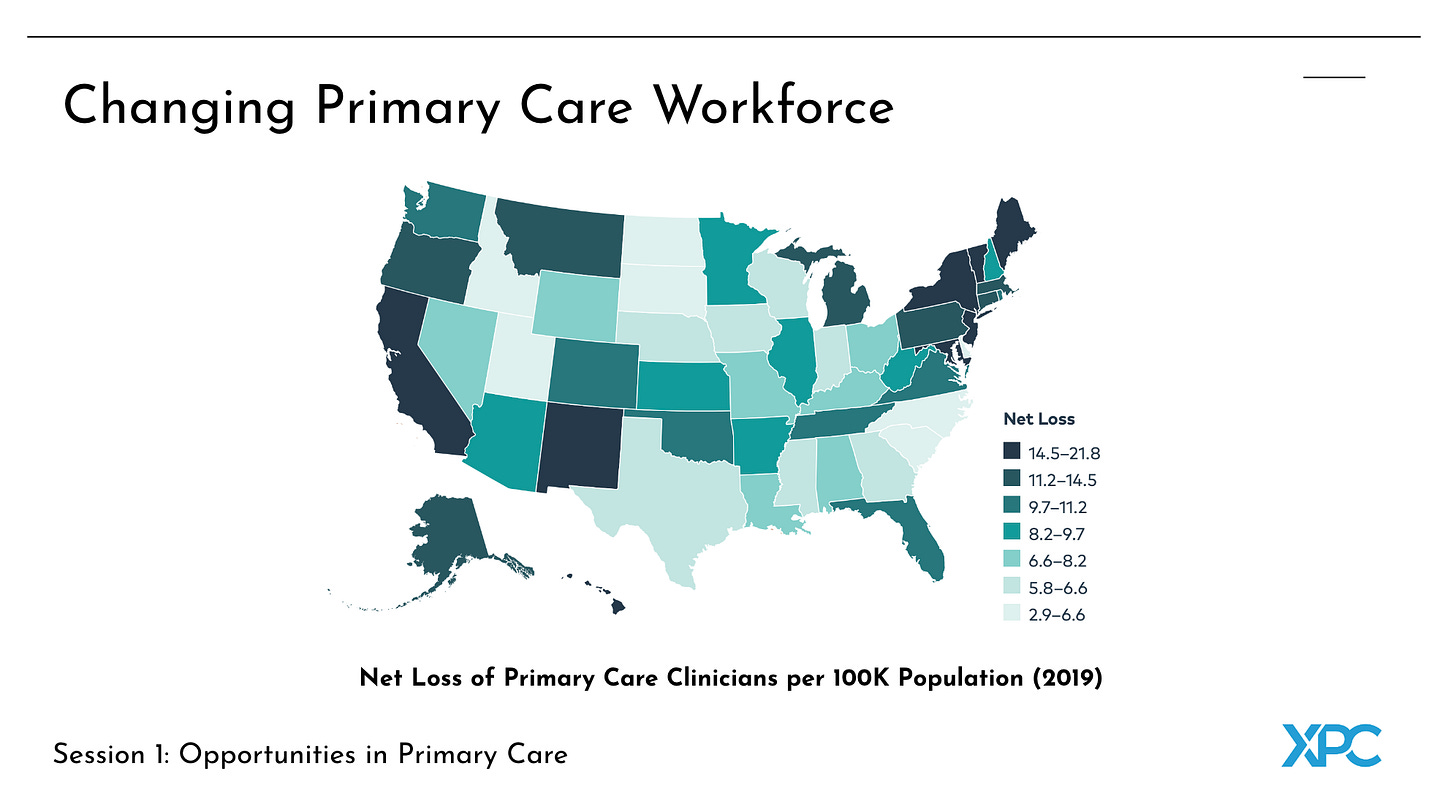
About half of all physician office visits happen in primary care. The concerning trend is the decreasing primary care workforce with a net loss of 10 clinicians per 100K people across the U.S. It’s troubling to see this because we have ample evidence that primary care delivers a high return on investment, with studies showing significant cost savings. For instance, a 2016 Oregon program documented that every $1 invested in primary care generated $13 in savings.
Between 1950 and the 1970s, the role of pharmacists expanded from dispensing medications to providing patient care services, reflecting a cultural shift within the pharmacy community. This led to the establishment of the PharmD programs, which particularly emphasized clinical education. The 1980s marked the beginning of the pharmaceutical care era, recognizing pharmacists as essential healthcare providers and leading to the universal adoption of the PharmD as the entry-level degree by 2005.
Becoming an ambulatory care pharmacist typically requires at least one year of postgraduate training, with additional certifications such as the Board of Pharmacy Specialties (BPS) or Board Certified Pharmacotherapy Specialist (BCPS) being helpful for job prospects. While it is possible to transition into this role without a residency, it usually requires more experience and connections.
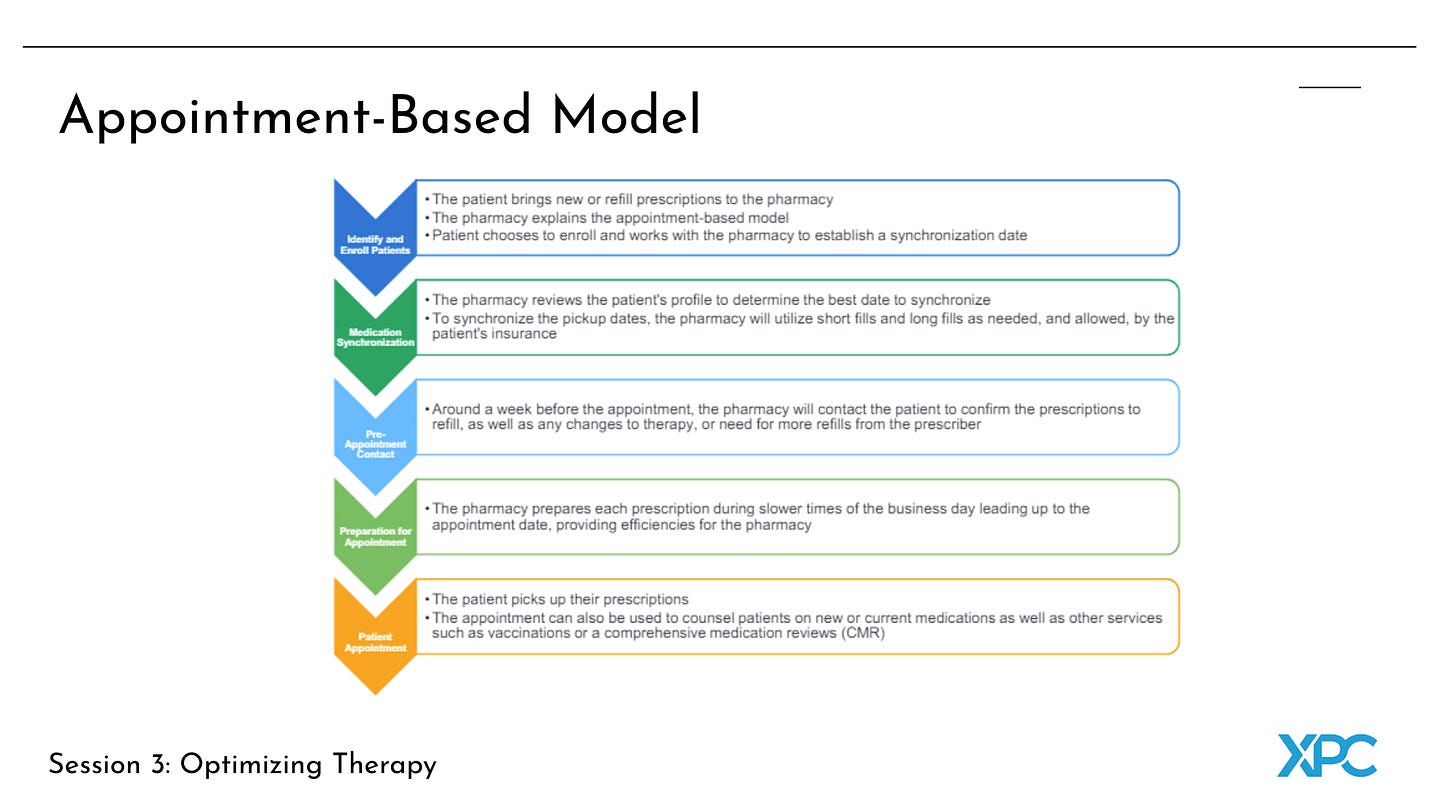
The appointment-based model is a program designed to improve medication adherence and provide efficiencies for pharmacies. This model combines medication synchronization with an appointment with the pharmacist, ensuring that all chronic medications are refilled on the same day of the month. The key difference between this model and an autofill program is the preemptive outreach to the patient before the appointment date to update any changes to their medications. The impact of this model can be significant, with medication adherence increasing by 20% or more, making patients 3 to 6 times more likely to adhere to their medication regimens.
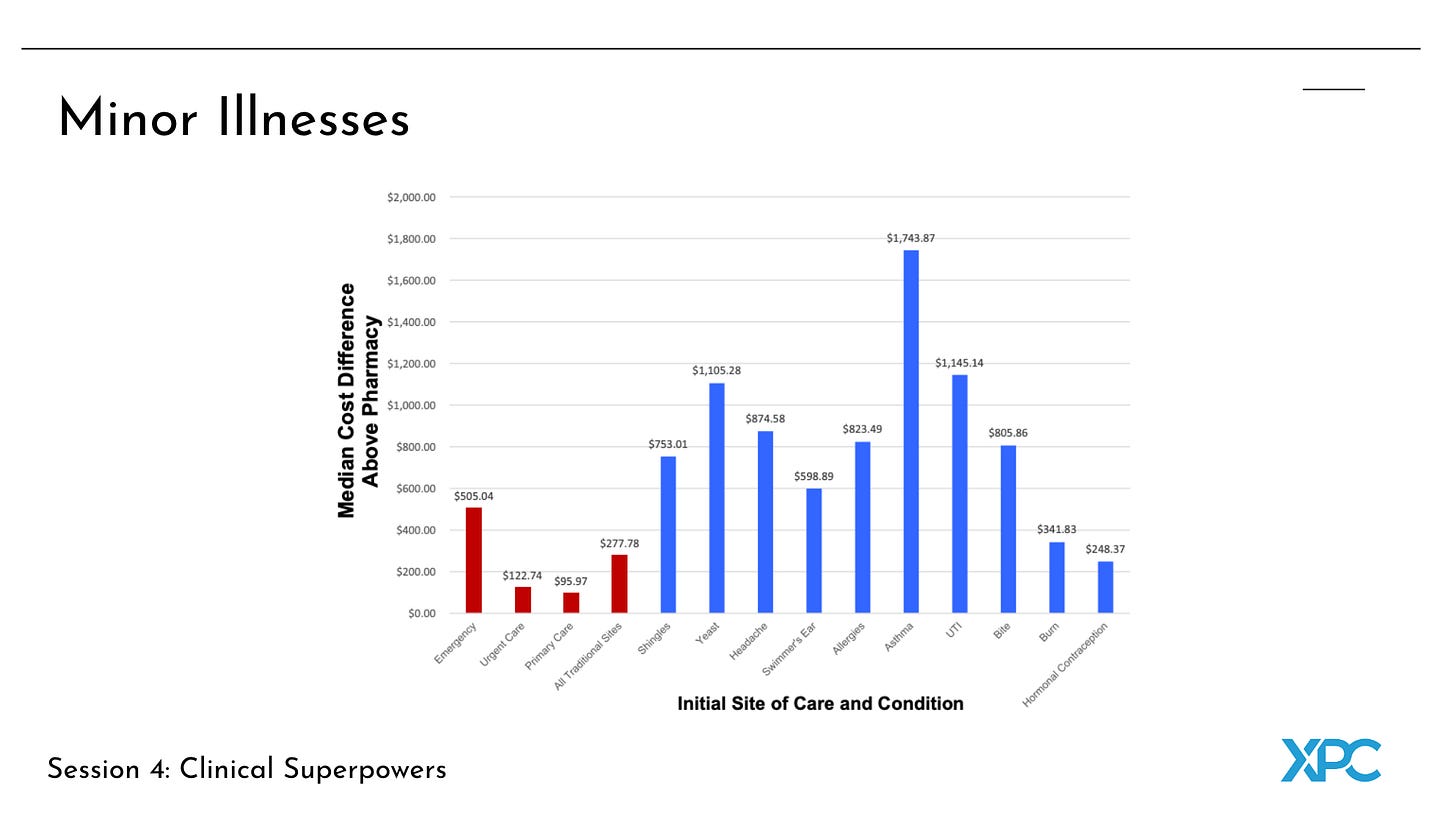
Pharmacists are also involved in point-of-care testing and the treatment of minor illnesses, which is particularly valuable for young adults and families who often seek urgent care for these conditions. For example, a program was set up in pharmacies where patients could receive a point-of-care test, have the results reviewed by a telehealth prescriber, and get a prescription while still in the pharmacy—all within an hour and at a lower cost than visiting an urgent care center. This model was found to save patients time and money, with the pharmacy visit costing about one-third of what an urgent care visit would cost.
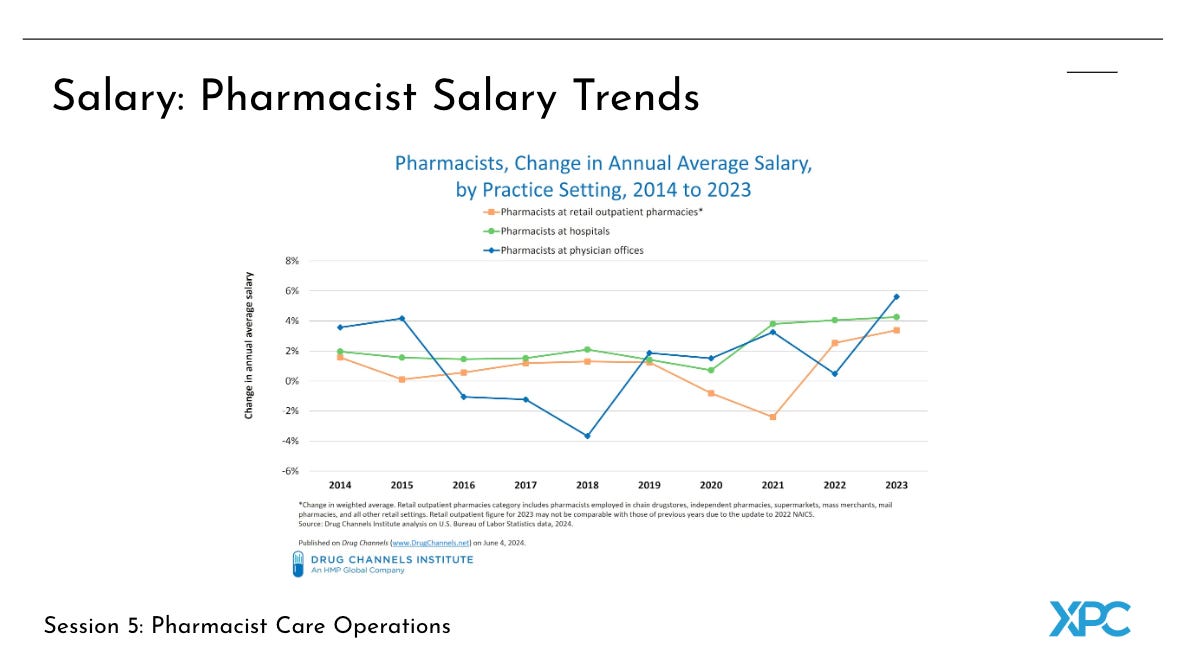
Pharmacist salaries in non-retail settings, such as physician offices, are often higher than those in retail or hospital positions. For example, in 2023, pharmacists in physician offices earned an average salary of $142,000. In contrast, nurse practitioners and physician associates generally earn slightly lower salaries on average (e.g. approximately $130,000), with those in physician offices earning below the overall average for their roles. The demand for pharmacists in clinical positions, particularly in physician offices, has been increasing, driving up salaries in these areas.
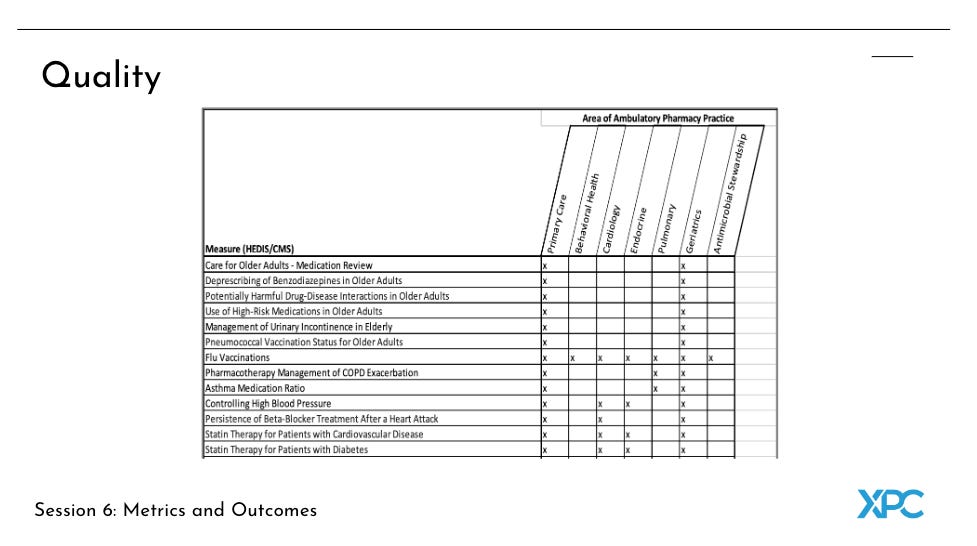
Pharmacists can significantly impact healthcare quality measures, such as those defined by the Healthcare Effectiveness Data and Information Set (HEDIS) and Centers for Medicare & Medicaid Services (CMS). Ambulatory care pharmacists contribute to improving outcomes in areas like hospital readmissions, emergency department utilization, and potentially preventable complications. They also help reduce fragmentation within the healthcare system by serving as a bridge between different care silos.
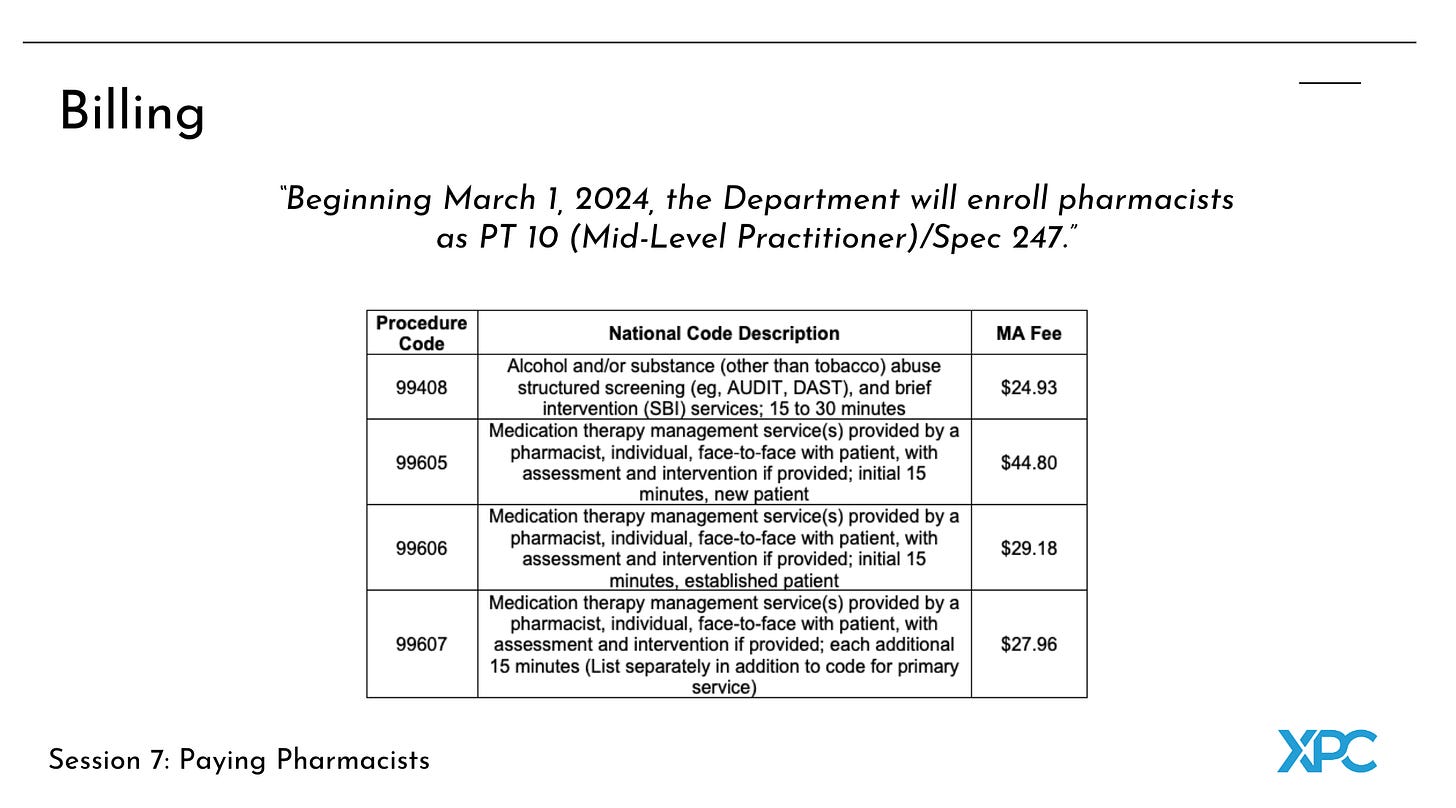
In some cases, pharmacists can bill directly for their clinical services. For example, since March 1, 2024, Pennsylvania Medicaid recognizes pharmacists as mid-level providers, allowing them to bill for services within their scope of practice. The list of billable services is extensive, covering everything from Hemoglobin A1c testing to vaccinations and patient evaluation and management.
Some private payers also allow pharmacists to bill directly for clinical services. Pharmacists must be credentialed, enrolled, and contracted with insurers to qualify for billing. Credentialing verifies the pharmacist’s qualifications and ensures they meet the necessary standards to join a provider network, which is essential for receiving reimbursement from health plans.
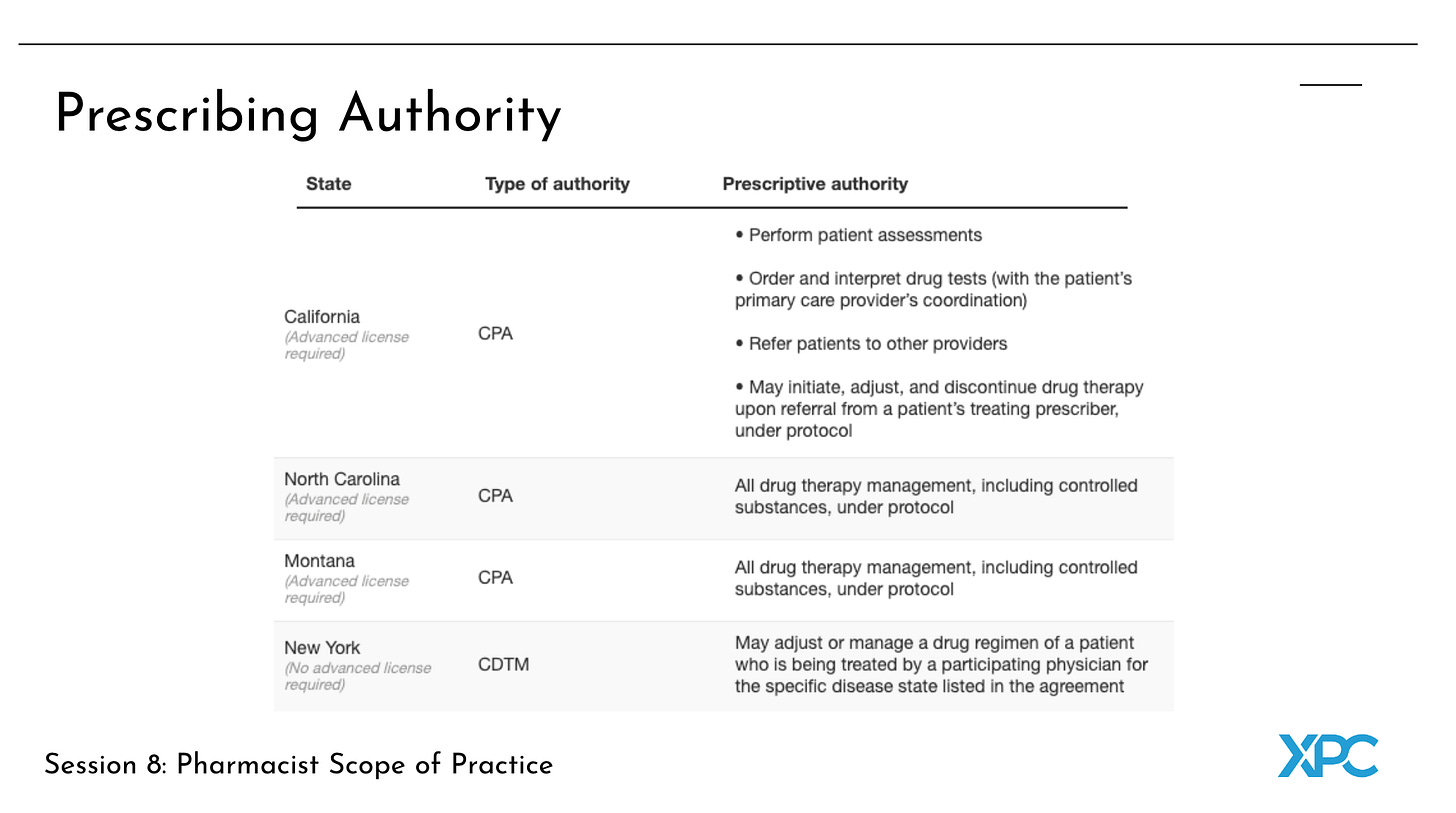
As of now, 18 states have CPAs that allow pharmacists to prescribe medications based on rapid diagnostic tests. If you look at prescriptive authority for pharmacists with an advanced license in California, they are able to perform the bread and butter services of primary care: “initiate, adjust, and discontinue drug therapy, order and interpret tests, manage diseases in collaboration with healthcare providers, and refer patients to other providers.”
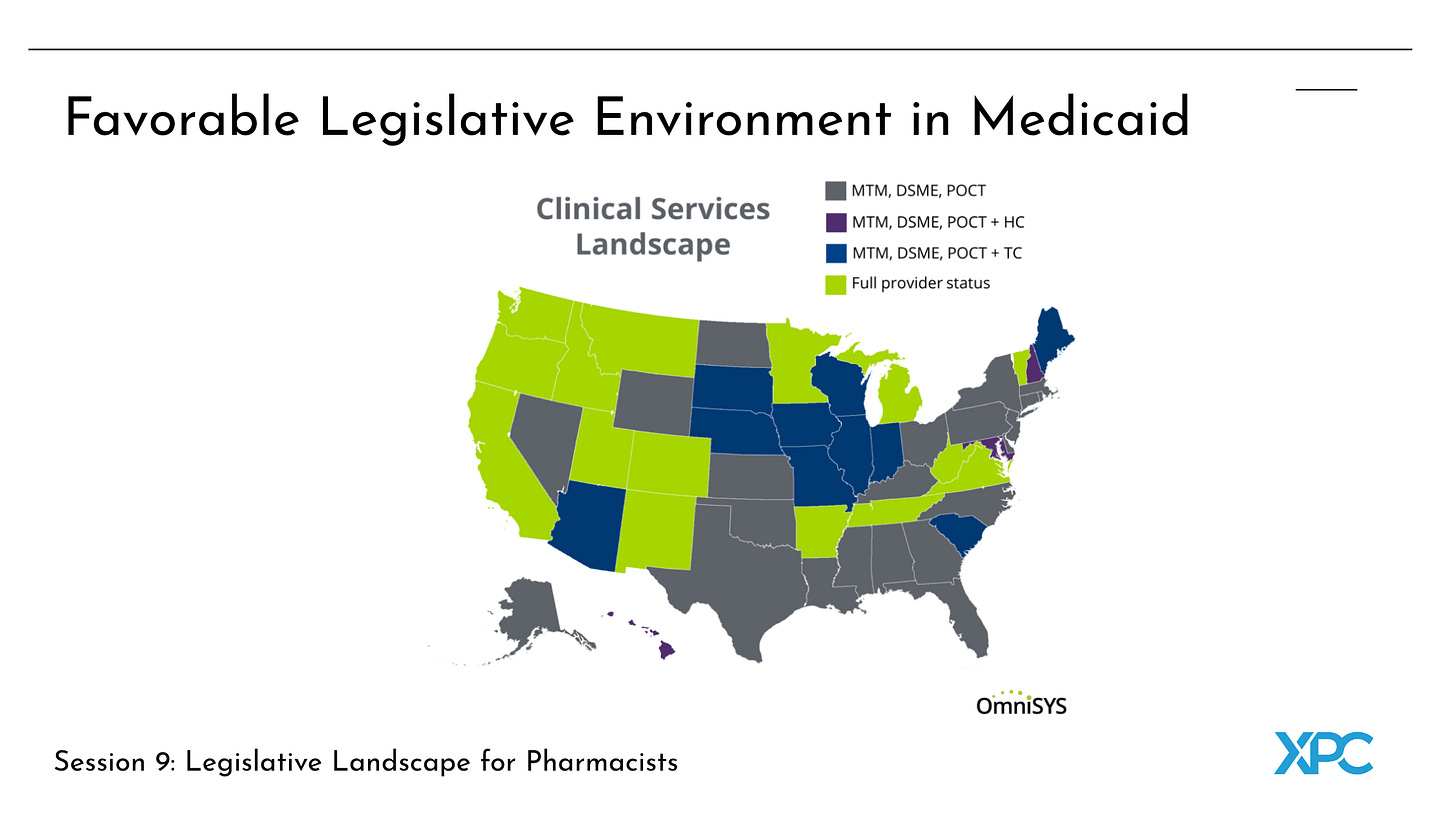
When evaluating favorable legislative environments for pharmacists, the key question is which states are willing to pay pharmacists for clinical services and recognize the full scope of their skills. Medicaid coverage for pharmacist services varies by state. Over 20 states have expanded Medicaid coverage to include pharmacist services, with 15 states granting full provider status, allowing pharmacists to bill for clinical services. Recently, Pennsylvania, New York, North Carolina, and Virginia have also offered pharmacist provider status.
Savvy primary care practice owners are beginning recognizing the immense potential of integrating pharmacists into their clinical teams. We predict that as practices scale, it will be common practice to bring on pharmacists as early hires over nurse practitioners or physician associates. The data and economics support this. Knowing how to operationalize this will be the differentiator for delivering high quality care. Reach out to us if you are interested to delve deeper into the topics we have covered.
P.S. XPC Clinic is open for collaborations 🚀






Your course has a great curriculum. Congratulations. In Brazil, the pharmacist has become very important in primary care too.