Rethinking Clinical Training
Why EMR simulations are the future
PSA: Applications are now open for the XPC Chart Biopsy Games from Feb 21-23, 2025. If you’re interested in clinical workflows and technology, apply now to reserve your spot.
How we learn to practice medicine has not changed in decades. It’s never been more exciting to reimagine how medical education and clinical training can catch up with modern practice. Here’s what drives my thinking about what’s needed and what’s possible.
Clinical experience gap is widening
Market trends are changing the healthcare workforce composition. Increasing numbers of seasoned physicians are leaving the profession while less experienced clinicians (e.g. APPs) backfill positions in demand. As a result, we have a growing clinical experience gap. On-the-job training is the current solution to make up for deficiencies in experience. For a deeper dive on these trends, read about the evolving primary care workforce and Bloomberg reporting on clinical training.

Chronic disease is ubiquitous yet rarely seen
Residency earned its name from an era when doctors lived in hospitals, learning medicine at their patients' bedsides. These patient cases were their textbooks, teaching them how diseases unfold from admission to discharge. This model excels for acute conditions like heart attacks and strokes, where immediate intervention is key. But modern medicine faces a different challenge: chronic diseases that develop over months and years, not days. The feedback loops in chronic care are painfully long—a medication change today might not show its full impact for months, and a missed intervention might not reveal its consequences for years. Even programs emphasizing continuity of care struggle to show trainees the full progression of chronic diseases. This training gap is particularly concerning given that chronic and mental health conditions consume 90% of US healthcare spend. Witnessing enough variations of chronic disease to build true expertise is nearly impossible through traditional training alone—it requires years of practice, patient by patient. And as our population ages, these conditions rarely come alone—clinicians must learn to recognize and manage complex patterns of interacting illnesses, often through trial and error with real patients (Figure 1).

Unlock EMRs as textbooks, not just QuickBooks
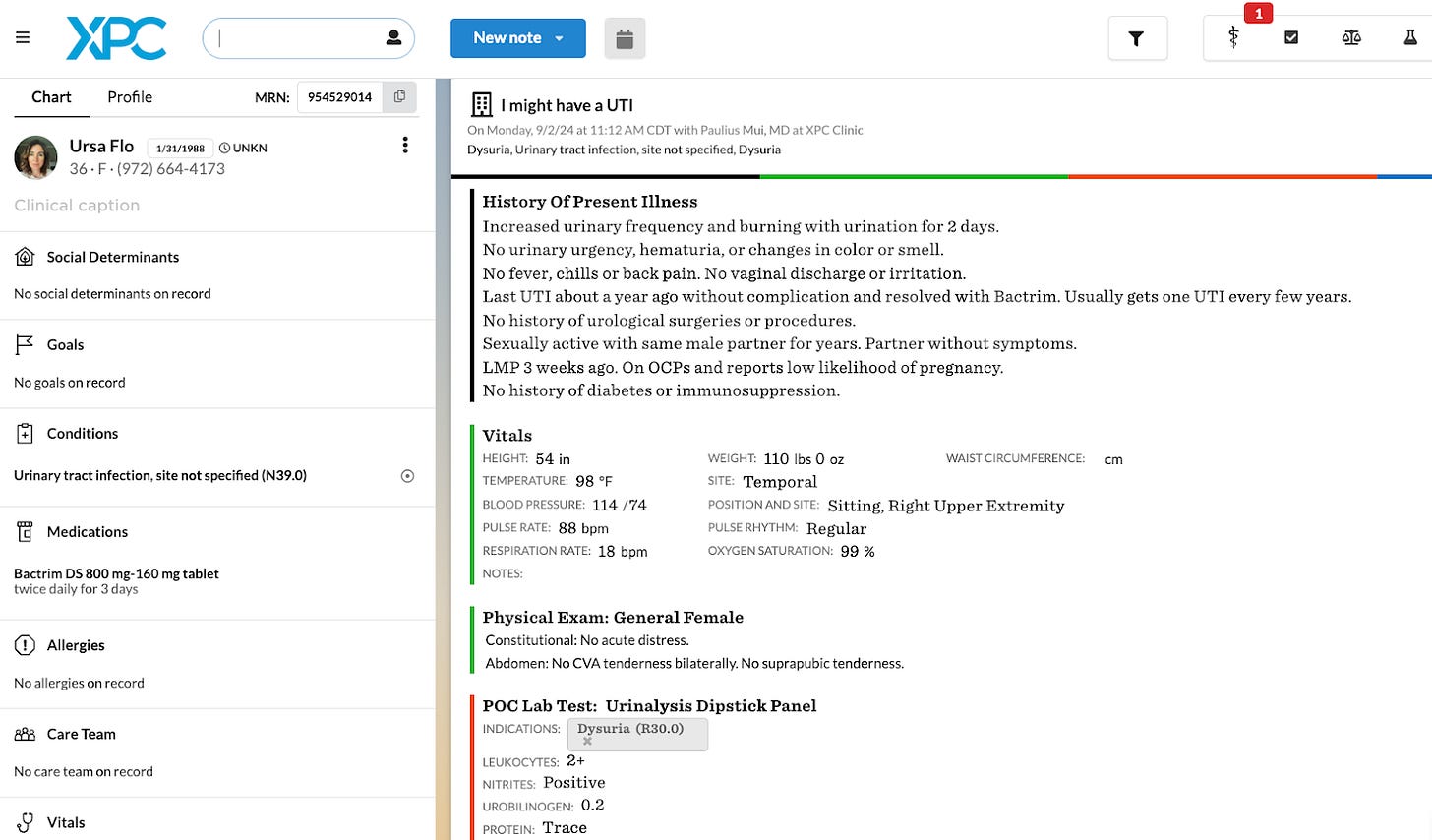
The Gutenberg moment for clinical training has been in front of us all along — the EMR (Figure 2). Yes, EMRs were designed for billing and are far from perfect. But beneath their administrative facade lies an untapped educational goldmine. Using medical records as a medium for curriculum delivery is not a novel idea yet nobody has seized this opportunity at scale. Creating and operating high-quality synthetic data to simulate patient care will be at the crux of the next revolution in clinical education. It’s only a matter of time before EMRs become adopted as the superior learning management system (LMS) in medical education. Data on trainee clinical excellence (e.g. prescribing behaviors, referral patterns) and operational excellence (e.g. productivity, inbox management) can guide training interventions. Insights about trainee readiness for the real world practice can inform hiring and placement decisions. Being able to benchmark and predict performance of their workforce will offer employers an advantage. More importantly, educational institutions may begin to differentiate by bearing risk on the quality of their graduates.
The market is beginning to notice this opportunity. Last year, Epic launched Lyceum to accelerate medical student adoption of their systems, while startups like EHR Go and Scope have created proprietary teaching EMRs to operationalize case-based learning. VCs are funding companies like Soma Lab (YC S24) to reimagine medical training through virtual clinical experiences. However, success hinges on seamless integration into real clinical workflows. Until (if ever) we free medicine from EMRs, that's where training needs to happen. In 2025, I anticipate a surge of capital deployment to tech-enable clinical training, driven by an urgent need: preparing the least experienced (and least expensive) clinicians who increasingly care for the most complex patients.
Breaking the specialist ceiling
Specialists master organs, but patients have illnesses that cross these boundaries. Today's training spreads generalists too thin across multiple domains, limiting their ability to develop deep expertise. EMR simulations could change this - enabling generalists to become experts in the chronic disease patterns their patients actually have. Just as some developing countries leapfrogged landlines straight to cell phones, EMR simulations can elevate generalists to hyperspecialists. By simulating years of disease progression in weeks, generalists can master the real chronic illness patterns in their communities (Figure 3). This precision training approach would advance health equity. Simulated care pathways can help drive targeted interventions for vulnerable patients (e.g. managing the interplay of obesity, schizophrenia, and COPD for a patient living in a food desert). For risk-bearing organizations, this means finally having a systematic way to train clinicians in the precise competencies that drive quality metrics (e.g. deprescribing anticholinergic medications in elderly patients to excel at Star measures).

More discovery ahead
There’s a strong signal for EMR-based simulations of chronic conditions to be the future of clinical training. This could be something that remediates low-performers already in practice, facilitates practice transformation (e.g. transitioning from FFS to VBC), differentiates candidates in the hiring process, platforms next-generation CME, or integrates with curricula of training institutions to measure trainee competencies.
P.S. If anyone wants to riff on additional use cases and GTM strategies, happy to share my findings from discovery work with ICPs as I build in this space. You can reach me at paulius@xprimarycare.com
Thank you to Alex Kazberouk and Emily Lu for reading drafts of this.



Great food for thought, just discovered this Substack and I love it!
A few thoughts:
Where I trained there were some efforts to use the EHR usage data as a tool to evaluate. There was lots of pushback though - to clinicians it felt a little big brothery. Nobody wants to feel like their clicks are being watched. This gets to the heart of a big problem in medicine - although everyone talks the talk about improving diagnostic error, quality, and cost, most physician groups will fight tooth and nail to prevent real data-based evaluations of their performance.
My other thought is about the long-term value proposition you’re proposing. If the emrs you’re imagining can become so good at teaching trainees how to care for complex and chronic disease, do we really need the humans to be so well trained in the first place?
Great read. Thanks for sharing. This could be interesting for CME and re-certification exams, too.